Is Your Horse Suffering from Undiagnosed Pelvic Fracture or Sacroiliac Strain?
- Elisse Miki

- Feb 4, 2024
- 18 min read
Updated: May 26, 2025
Back (sacroiliac) pain is arguably the most common finding in equine athletes at an astounding estimate of up to 94% of ridden horses affected [14]. If there is data indicating this prevalence then it begs the question why many equine profressionals neglect to undertake a complete orthopaedic examination.
To date there has been no large-scale study of the clinical signs of sacroiliac (SI) joint pain and its association with lameness and/or thoracolumbar pain [15]. Considering the mulitude of research in this area for humans and the alarming statistic above regarding prevalence, this finding is disturbing.
We need to do better as professionals.
Research is highly lacking in the equine industry.
In order to raise the bar to the level of standard that human patients experience, global awareness towards stricter regulation of equine professionals is required.
Often we see massage or other forms of bodywork applied without full orthopaedic assessment undertaken. This is not only unethical, it is dangerous.
Undiagnosed pelvic fracture and sacroiliac strain are more common than one may think. Many will go undiagnosed for weeks, months, years, or even a lifetime for some horses.
In this blog
I share with you two of the most shocking cases I had the privilege of assessing this past year. What you will discover, as I did, is that these horses all received extensive veterinary diagnostics, treatment, and prior manual therapy interventions with no resolve. Not because the fracture or strain did not heal but because it was not identified in the first place.
First, a little bit of anatomy to orient you with the involved structures.
What is the pelvis and pelvic ring?
The pelvis connects the hind limbs to the spine via the hip and the sacroiliac joint.
The pelvic ring is made of the sacrum and two innominate bones, each containing an ilium, ischium, and pubis [1]. There is minimal inherent stability to the bony anatomy of the ring, therefore strong ligamentous attachments are required for maintaining balance and structure [6].
Image 1: Caudal View: 1) innominate bone 2) sacrum 3) hindlimb 4) SI Joints
Image 2: Cranial View: pelvic ring
When there is a pelvic fracture there will be concurrent sacroiliac strain of the supporting ligaments due to the distinct articulations of the pelvis. It is equally possible (and common) to have a sacroiliac strain occur independant of pelvic fracture.
What is the sacroiliac joint?

The sacroiliac joint (SIJ) is a synovial joint, which means it has a joint capsule around it to provide stability and protection. Normal physiology of the SIJ dictates that it is designed primarily for stability with only minimal available mobility [5], hence interventions should not willfully seek to increase range of motion at this joint beyond physiological barriers through injections or any other invasive practice.
What are the functions of the pelvis?
1. Locomotion
The pelvis allows for motion and force produced by the hindlimb to transfer through the spine and create what we see as hindend movement. The sacroiliac joint is the primary joint that connects the hindlimb to the spine and facilitates this process by absorbing and dissipating force and load vectors.
2. Protection
The pelvis houses vital organs, blood vessels, and nerves. Primary organs include digestive and reproductive organs which are essential for life sustaining processes, The main blood and nerve supply for the entire hindlimb exits through the pelvis. This is why it is surrounded and infused by very dense muscle and fascial tissues. These organs include bladder, rectum, and part of the colon. In females, the pelvis also houses the uterus, fallopian tubes, and ovaries. In males, the pelvis also houses the ductus deferens, seminal vesicles, ejaculatory ducts, and prostate.
3. Muscle attachment

The pelvis provides firm attachment sites for the major muscles responsible for movement and stability such as the gluteals, hamstrings, and hip flexors. The muscles of the pelvic floor also line the internal surface of the ring and facilitate healthy waste product removal and hormonal function.
4. Birthing
In the female horse, the pelvis facilitates opening of the birth canal to allow passage of the baby.
How does injury impact the horse?
If any one bone of the pelvis or sacroiliac joint is injured, effects will be widespread. Symptoms are definite in any structure that is neighbouring, either ahead of (i.e. the spine) or below the level of the fracture (i.e. hip, stifle, hock, distal limb). This is due to the fact that functional mechanics of the pelvis dictates how the entire limb and spine will move (or not move). What this means is that we can see pain and dysfunction in multiple neighboring structures as well as very distant to the site.

Even a simple tear in the ligaments holding the SI joint togethers can produce profoundly catastrophic pain and dysfunction. Ask any human who has injured their SI joint.
What causes pelvic fracture and/or sacroiliac strain?
Pelvic fractures and sacroiliac strains (commonly referred to as subluxation) are usually associated with impact trauma which includes falls and collisions [1]. In senior horses, much like humans, accidental slips, falls, or small impacts, can be enough to cause damage if bone density and joint integrity is compromised [10].
How are they typically diagnosed?
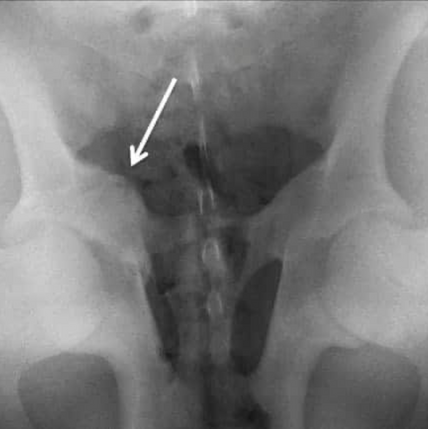
Hairline fractures (also known as stress fractures) are among the most challending to identify due to imaging limitations. MRI and/or bone scintigraphy are the preferred diagnostic modality for humans [2] because these types of fractures do not always show up on X-Rays or ultrasound, which begs the question, what about our horses?
In areas lacking access to advanced veterinary technology or insurance funding it is important to recognize the insuffiency in diagnostics this presents.
Ultrasound or X-Ray may be the next best diagnostic option, however, are not always conclusive depending on size and fracture location.
Internal palpation may be used to identify gross changes in anatomy but unfortunately many hairline fractures are not easily palpable. This is why careful evaluation of the horse's signs and symptoms alongside qualified veterinary and paraprofessional assessment can provide the owner with valuable insights.
What are the signs and symptoms?
In the acute stage, meaning it just happened, pelvic fracture can mimic a distal limb injury as the horse will likely be unable to bear weight thought the affected limb and swelling may pool in the extremities. There will be obvious pain. This can present similar to a distal limb injury when in fact it is not.
In the sub-acute and chronic stage, meaning a few weeks to months later, we will begin to see more issues in the limb(s) compounding the presentation. Think back pain, stifle pain, hock pain, suspensory issues, flexor tendon issues, hoof issues, and compensatory movement strategies. Additionally, we will likely begin to see dysfunction into the forelimbs and head and neck from long term compensation. In this stage we will observe movement limitations showing up as inability to pick up canter leads, bunny hopping, disuniting, and a various feedback from the horse; lack of motivation to move forward, depression, frustration, irritability with movement requests (i.e. bucking, rearing, bolting).
Image on left example of acute stage presentation
Image on right example of chronic stage presentation
A common sequel to pelvic fracture and/or SI strain is lower back pain and disorders such as kissing spines. These tend to present in the later stages of fracture or SI strain healing, especially when the original injury was not identified in the first place.
The relationship between changes in dynamic loading through the vertebral joints following pelvic injury is well understood and seen consistently in human practice yet often overlooked in the evaluation of the equine patient despite research efforts [7]. Human studies are even constructed around the understanding that pelvic orientation and/or injury can predispose the body to specific degenerative spinal pathologies [3].
A thorough understanding on anatomy and physiology of joint motion can quite easily demonstrate the interdependant relationship of the spinal column with the pelvis as is seen in human practice [8]. One must only explore the many texts and resarch articles pervading human therapies to recognize the frequent lack of scientific method application in the equine industry.
Many owners mistake back pathology to be primary when in fact it is secondary to a pelvic fracture and/or sacroiliac strain. This is also often when the vet is called as the horse may be presenting with aversive symptoms of back pain.
Either singularly at first but over time multiple structures may become involved. These impacts are predictably notable, moreover a matter of when this will impact the horse rather than if. Most owners will recognize their horse's presentation as atypical but diagnostics are often inconclusive if only the peripheral limb is examined.
Furthermore, once the original injury has healed, radiographic evidence will no longer be identifiable. This can further compound the confusion around findings at that time as pelvic fracture and SI strain predispose the horse to distal limb pathologies such as flexor tendon and suspensory tears, sesamoiditis, and arthitis to name a few.
Case Study: Let's look at a human example....
This is a case example that was treated in my human practice. Patient, 36yr old female, had a fall from a 6-ft ladder. Reported landing with all weight onto one leg in an attempt to break the fall before tumbling onto her side. She reported there was sharp pain immediately and that she was not able to put weight through the affected leg. The patient went to the doctor the next day and was sent for X-Ray imaging which came back clear for fracture of the femoral neck. No imaging was taken for the pelvis. She was instructed to rest and take NSAIDs for the next 4-6wk.
Nine months later patient is able to functionally stand up or walk but has returned to working at her desk job. She had also resumed activities of daily living (driving, cooking, cleaning) but had not been able to return to exercise (running, biking, gym) due to persistent pain in the lower back and knee of the affected leg. The patient was taking between 6-8 doses of NSAIDs daily with reports of pain remaining between 7/8 out of 10. This is when she came to my office for assessment and treatment.
Orthopaedic assessment findings revealed what is termed a pelvic upslip. This is where the ilium has slipped "up" on the sacrum which means she had suffered sacroiliac strain.
Furthermore, fibrosis and dense scar tissue consistent with a post hairline fracture site was palpated at the lateral side of the hip. There was pain and limited range of motion (actively and passively) in the lower back, hip, knee, and ankle on the affected side with the unaffected side demonstrating similar limitations but milder pain.
This case is an example on how the body has the ability to compensate an injury in the short term but over the longer term and even once the soft tissues are healing/healed there will still be pain due to altered biomechanics and the presence of scar tissue. This compensatory movement strategy places stress and strain on other structures such as the lower back, knee, ankle and contralateral limb and is a major predisposing factor for other pathologies such as spinal degeneration, arthritis, and tendinopathies in the major muscles of the upper and lower leg.
This patient, was referred by myself back to the doctor for imaging based on positive presentation for concurrent spinal pathology. Testing came back positive for arthritic changes in th SI and lumbosacral joint and positive for compression with nerve impingement in the lower back. This patient had no history of back pain or injury prior to this fall and was generally very healthy and fit.
Without the ability for the human patient to speak and provide us with the integral case history (i.e. I had a fall and I am still in pain nine months later), we would only have a full orthopaedic assessment to provide us the pertinent information needed to create a relevant treatment plan.
This is why we must assess the whole horse rather than solely peripheral limbs.
If this is so simply understood and treated in human practice then why not the same approach for our horses?
This level of assessment process was required for board examination in my human licensing. It was not an option to forego the study and a large part of the reason we maintain our regulation as health care professionals (in Canada).
Next lets look at the equine cases from my practice...
Case Example #1
Horse had a suspected fall in paddock when the ground was frozen. At onset of injury the horse was unable to weight bear on the affected limb. The veterinarian was called and diagnosis concluded left stifle injury following an ultrasound and bilateral hock X-rays. Treatment for the stifle included PRP (stifle), corticosteroid injections (hocks), Legend injections, rest, and Bute.
9 months later the horse continued to decline and the owner called me to come assess for proposed underlying soft tissue dysfunction. Included below are the most pertinent assessment points, however, a complete head to hoof orthopaedic evaluation was undertaken which was consistent with the forementioned notes.
This was the mare's preferred standing posture observed following multiple trial of walk-halt and asking to square
Pelvic orientation severely asymnetrical indicating SI strain (dissassociation of ilium from sacrum).
From the posterior view, severe displacement of the right side pelvic bones > 3-5mm.
Note: asymnetry greater than 3-5mm in human practice is consistent with displacement/disassociation of the SI joint. This condition is usually due to trauma such as a fall wherein fracture is consistently correlated. When this degree of asymnetry is observed, it is considered indicative of an acute traumatic event rather than general soft tissue imbalance such as "tight muscles".
From the side view, cranioventral (towards the ground and head) displacement of the left ilium and offloading of the limb as seen in the weight shift to the toe and stepped back.
In gait, the key areas noted above are clearly illuminated (pre-post session videos below). Identifiable asymnetrical loading patterns with global compensation as seen in the diagonal walking mechanics and bracing of tail (sacrum). Strain to all structures below the level of the pelvis bilaterally in opposing parameters. When joints are loaded outside of their normal physiology accessory movements in the distal joints is concurrent as seen in the pre-session video.
This certainly predisposes the horse to injury and pain of distal joints, as the stifle diagnosis indicated.
At a trot this horse was lame.
Following our first session, below are the changes to standing posture and gait. These improvements were following only one 60min manual therapy intervention. The working hypothesis included a potential for post-pelvic fracture with obvious subluxation of the pelvic bones (ilium from sacrum) and was treated as such. This horse's managment plan included future monthly sessions and homecare consistent with human therapeutic protocols.

This case dramatically highlights the value in thorough assessment and the adaptability of soft tissues towards a desired positive outcome. Changes this phenomenal are common practice when thorough assessment is undertaken in the first place. This horse is now (one year later) back to functional activity which includes groundwork and trail riding.
Case Example #2
Owner purchased horse in June 2020. Three months later, owner called the vet due to structural issues (lack of topline), visceral concerns (freqent defecation) as well as difficulties with movement (cold backed, canter transitions). Veterinarian diagnosed horse with Kissing Spines.
Professional saddle assessment and adjustment was completed and horse started being ridden a few days a week.
The horse continued to decline. Further Veterinary treatment inlcuded multiple rounds of steroid injections to the back and a prescription for Gastrogaurd. Following this series of treatments and time off, the horse became unrideable.
At 3 months post Kissing Spines diagnosis, the horse received a series of 12 laser treatments to the back in conjunction with monthly bodywork and bi-monthly PEMF. He was also put on a core conditioning program, including pole work and stretches which would continue for the next year.
At one year of rehabilitation the horse received one session of Shockwave Therapy to the back and presented with a sharp increase in pain following the session and was deemed unrideable indefinitely. From this point, the owner solely lunged the horse for another 6 months.
The horse continued to decline and was referred for spinal surgery to shave spinous processes and perform longitudinal snips on the supraspinous ligament. In humans, when this ligament is cut there will be a moderate to severe reduction in spinal function due to its interdigitations with the nuchal ligament and primary role in spinal stabilization and force absorption [16].

Note: the supraspinous ligament is designed to stabilize the neck and back. One of its roles is to maintain the head in upright position. It is stretched in flexion, and it`s fibers resist separation of spinous processes during forward flexion. During hyperflexion interspinous ligament and supraspinous ligament are the first to fail (i.e. tear = sprain) [12]. Sprain of the supraspinous ligament (whether intentional such as Shockwave therapy or not such as injury) can cause acute back pain, pain on palpation, atrophy of longissimus dorsi, and altered gait [13] seen as lamenesss and/or head drop to ground posture due to lack of stability to maintain head upright.
Following surgery, the next rehabilitation program included, 1month stall rest with daily walks, followed by 1mo paddock turnout with daily walks, then begin of lunging at 3mo.
During this time, the horse was observed to lack balance and co-ordination. He experienced falls while working on ground which appeared to be due to the hind end "giving out" and presented with general lack of proprioception in bilateral hinds. The horse was re-evaluated by the Veterinarian in March 2023 and sent for a bone scan and further X-Rays.
The bone scan report indicated minimal to mild dorsal process remodeling present between T12-18 and mild arthritic changes in hocks and fetlocks. X-Rays for hocks and cervical spine came back with no additional comments or suggestions. Owner next tried another series of alternative treatments including mesotherapy, acupuncture, steroid injections, NSAIDs, red light.
At this point, reaching over three years of attemped rehabilitation, the horse was still presenting with severe pain and unrideable.
Plans were made to retire him up country but the owner decided to make one last attempt at obtaining some answers. This is when she reached out to me for an orthopaedic evaluation.
Some of the answers are right in front of us
In collecting extensive case history information in advance, it is clear that there were many red flags present for which assessment needed to provide clarification. Upon reading this horse's intake form and recieving copies of previous imaging, I sat down with the owner to gather refining information.
Owner Observations
"When I got him, he always needed to be lunged first as he presented as quite cold backed. We were in a regular weekly lesson program doing WTC, however, he had troubles maintaining canter both on the lunge line and under saddle, especially to the left."
"I noticed that the top right side of his illium seems to be about 1/2cm higher than the left. I don’t know how long it has been that way but he has looked this way since I got him."
"He always has and still remains quite tight with his right hind, holding it very close to his body and remains reactive in the muscles around the sacroiliac region."
"Both before and after surgery he has had a tendency to work (both on lunge and u/s) with his head in the dirt, mainly at trot and more evident going to the left."
"He responds quite negatively to any of the more robust medical treatments he has had done, ie. steroid injections along the dorsal ligament, the shock-wave therapy, acupuncture with electrodes and Mesotherapy. He does, however, react quite positively to physio and PEMF treatments, but they only seem to last a short time."
"Is very sensitive to saddle placement and if it slips forward into his shoulders, he would stop dead and not move."
Red Flag
When did this pelvic asymnetry begin to present?
The owner reported that he had come with this sharp asymentry that was visible from behind. When asked if he had a fall, she was unsure of his prior health history but remembered the previous owner reporting an undiagnosed lameness prior to purchase.
Based on pelvic presentation at the time that of my assessment, the tissues appeared to be well into a chronic state (i.e. it happened a long time ago).
Assessment
Following case history review, observation, gait evaluation, and range of motion testing were completed and it became quite obvious there were many answers right there in front of us.
Included below are the most pertinent assessment points. Complete head to hoof orthopaedic evaluation was undertaken which was consistent with the forementioned notes.
This was the gelding's preferred standing posture observed following multiple trial of walk-halt and asking to square. Pelvic orientation severely asymnetrical (> 3-5mm).
From the posterior view, severe asymnetrical loading. Weighting to the left, offloading the right. Stands with narrow base of support and bilateral external rotation of hindlimbs (indicates SI and hip dysfunction). While this photo appears to be taken on a sideways plane, it is suprisingly not. This is how the horse chose to stand upon repeated walk to halt transition.
From the side view, weighted onto hind toes and bilateral forelimbs extended (standing parked) indicating offloading of thoracolumbar spine. Atrophy in paraspinal and cervical musculature and lacking development in thoracic sling. Moderately high head position in static standing.
In gait, the key areas became more clearly illuminated. Asymentrical loading and compensatory movement strategies (pre-post session videos below). Similar to the previous case, visible asymnetrical loading patterns with global compensation as seen in the diagonal walking mechanics and bracing of tail (sacrum). Strain to all structures below the level of the pelvis bilaterally in opposing parameters.
Similar to the previous example, this movement strategy will predispose the horse to pain an injury of the hip, stifle, distal limb joints, and associated tissues. Affects of these altered mechanics will also travel through the spine and were concurrently reflected in the spinal examination.
Another red flag moment during this horses's assessment was the trot evaluation on a circle. The horse demonstrated attempted offloading of spinal segments seen in the excessive nose to ground strategy. This is not normal physiology and is usually indicative of spinal pain and dysfunction. Considering this horse's supraspinous ligament was snipped without rehabiliation of the proposed pre-existing pelvic dysfunction, spinal stability was severely compromised. Remember: one of the role of the supraspinous ligament is to prevent excessive spinal flexion.
Following 5 x 60min manual therapy sessions, below are the changes to standing posture and gait. The working hypothesis included potential for post-pelvic fracture with subluxation of the pelvic bones (ilium from sacrum) and was treated as such.This horse's managment plan also included future monthly sessions and homecare consistent with human therapeutic protocols.
Within One Session:

Results
Improvement in symmetrical loading of pelvis reflected through increased base of support towards neutral and decreased weight shift to left
Still demonstrating bilateral external rotation of limbs to be treated over course of next sessions
1mo Follow Up:
Results
Improved symmetrical loading
Reduction in asymetrical hip drops
Decreased deviation to the left, global diagonal pattern reduced
Tail head reduction in brace (sacrum gaining mobility)
5mo Follow Up:

Results
Less steep spinal angle at mid-thoracic spine (decreased compresssion intervertbral joints and corresponding nerves)
Improved musclulature neck (less inverted)
Improved activation of thoracic sling (sternum less dropped through forelimbs)
Less spinal brace (tone, texture, tenderness of paraspinal muscles)
Head set closer to neutral
6mo Follow Up:

Results
Thoracolumbar spine improved alignment (less excess extension)
Ability to hold spinal posture on own
Improved muscle development (paraspinals)
Increased range of motion bilateral hindlimbs (able to more easily step forward and under)
Reducation in nose-to-ground offloading strategy
Change is Necessary
If licensend human therapists are required to undertake such extensive orthopaedic evaluation which is board examinable, then why is this same science unapplied in equine therapeutic practice?
If human studies are able to demonstrate clear mechanical relationships, then why does this seem to be unchartered territory in mainstream equine science?
Does this sound reasonable to you. It does not to me.
In order for fewer horses to suffer from lack of thorough evaluation, there must first be awareness of the relationship between orthopaedics and pathology.
Commonly we will also see injections administered without any intervention for the displacement of the pelvic bones. Without re-orientation of bones and joints, injections will only further destabilize an already destabilized joint. More on injections in a future blog!
In Conclusion
The prevalence of pelvic fracture and/or SI strain is substantially more common than many believe. While I have only shared with you two cases from the previous year, rest assured I have seen this presentation in approximately 25% of my equine caseload. That is an astonishing one in four horses.
The science is there in human studies. Now it is time to do better for the horses.
My first horse put me on this path by entering my life with a pelvic fracture and subsequent sacroiliac strain. His injury was undiagnosed until I was able to obtain the relevant imaging and complete a full orthopaedic assessment. He taught me the critical importance of careful and complete evaluation before making determinations. He also showed me that functional recovery and rehabiliation is possible when we are treating the appropriate pathology.
Ready to Learn More?
Explore our Free Resources for tools you can use right away, dive into our Online Courses to deepen your knowledge, or join one of our Certification Programs to take your equine therapy practice to the next level.
Works Cited
1. Budras, K.-D. (2012). Chapter 9. In Anatomy of the horse (pp. 72–73). essay, Schlütersche.
2. Tins, B. J., Garton, M., Cassar-Pullicino, V. N., Tyrrell, P. N., Lalam, R., & Singh, J. (2014). Stress fracture of the pelvis and lower limbs including atypical femoral fractures—a review. Insights into Imaging, 6(1), 97–110. https://doi.org/10.1007/s13244-014-0371-z
3. Strube, P., Pumberger, M., Sonnow, L., Zippelius, T., Nowack, D., Zahn, R. K., & Putzier, M. (2018). Association between lumbar spinal degeneration and anatomic pelvic parameters. Clinical Spine Surgery: A Spine Publication, 31(6), 263–267. https://doi.org/10.1097/bsd.0000000000000660
4. Haussler, K. K. (2011). Diagnosis and management of sacroiliac joint injuries. Diagnosis and Management of Lameness in the Horse, 583–591. https://doi.org/10.1016/b978-1-4160-6069-7.00051-1
5. Degueurce, C., H., & Denoix, J.-M. (2010). In vitro assessment of movements of the sacroiliac joint in the horse. Equine Veterinary Journal, 36(8), 694–698. https://doi.org/10.2746/0425164044848064
6. Perry K, Mabrouk A, Chauvin BJ. Pelvic Ring Injuries. [Updated 2022 Sep 25]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544330/
7. Jeffcott, L. B., Dalin, G., Ekman, S., & Olsson, S. ‐E. (1985). Sacroiliac lesions as a cause of chronic poor performance in competitive horses. Equine Veterinary Journal, 17(2), 111–118. https://doi.org/10.1111/j.2042-3306.1985.tb02063.x
8. Cook, G., Burton, L., & Torine, J. (2017). Movement: Functional movement systems: Screening, assessment, and corrective strategies. On Target Publications.
9. DonTigny, R. L. (1990). Anterior dysfunction of the sacroiliac joint as a major factor in the etiology of idiopathic low back pain syndrome. Physical Therapy, 70(4), 250–262. https://doi.org/10.1093/ptj/70.4.250
10. Riley R. Accidental falls and injuries among seniors. Health Reports. 1992 ;4(4):341-354. PMID: 1306354.
11. Goodman, C. C., & Fuller, K. S. (2009). Soft tissue, joint, and bone disorders. In Pathology: Implications for the physical therapist (pp. 1294–1317). essay, Saunders Elsevier.
13. Higgins, A., Snyder, J. R., Macdonald, M. H., Kannegieter, N., Peroni, J. F., & Merfy, Wm. E. (2006). Chapter 15: The musculoskeletal system. In The equine manual. essay, Elsevier Saunders.
14. Haussler, K. K. (1999). Chiropractic evaluation and Management. Veterinary Clinics of North America: Equine Practice, 15(1), 195–209. https://doi.org/10.1016/s0749-0739(17)30172-4
15. Barstow, A., & Dyson, S. (2015). Clinical features and diagnosis of sacroiliac joint region pain in 296 horses: 2004–2014. Equine Veterinary Education, 27(12), 637–647. https://doi.org/10.1111/eve.12377
16. Merter A, Karaca MO, Yazar T. Biomechanical effects of sequential resection of the posterior ligamentous complex on intradiscal pressure and resistance to compression forces. Acta Orthop Traumatol Turc. 2019 Nov;53(6):502-506. doi: 10.1016/j.aott.2019.08.016. Epub 2019 Sep 16. PMID: 31537433; PMCID: PMC6939010.
Images Cited
Pelvic Bones
Equine Pelvis
Pelvic X-Ray
Pelvic Fracture
Kissing Spine
Acute Injury
Chronic Injury
Sacroiliac Ligaments & Muscles
Supraspinous Ligament


























Comments